 Measuring program value, or return on investment, is critical and imperative in managing a healthy wellness program. Further, clearly identifying and objectively evaluating the impact helps keep the vendor focused on what is critical for the employer. If these programs are not having the impact intended, then the cost of those services is only adding to medical spending waste.
Measuring program value, or return on investment, is critical and imperative in managing a healthy wellness program. Further, clearly identifying and objectively evaluating the impact helps keep the vendor focused on what is critical for the employer. If these programs are not having the impact intended, then the cost of those services is only adding to medical spending waste.
When adding wellness services to any employer benefits package, it is imperative to clearly identify the intended impact and outcome. Outcomes fall into three general categories:
- Employee satisfaction with the employer, which adds to recruitment and retention
- Reducing biometric risk and improving the health of the population
- Reducing medical spending
Employee Satisfaction
In the book, Shared Values, Shared Results by Dee W. Eddington, Ph.D., and Jennifer S. Pitts, Ph.D., the value of employees appreciating the benefits an employer offers is clearly outlined as a win-win strategy. If an employer’s intent in providing wellness services is to improve the support for its employees, then measuring the satisfaction related to those outcomes is critical. Employee surveys are typically the best approach to gather outcomes related to these intended programs. Some key questions to ask may include:
- Is working at this organization beneficial for my health? (“Strongly Agree” to “Disagree” responses)
- Do I trust that my organization cares about me? (“Strongly Agree” to “Disagree” responses)
- Which of the following wellness program initiatives do you find to be valuable? (list all programs offered)
Collecting employee, or spouse, feedback on these programs will provide insight to allow an employer/ consultant to know if programs are appreciated, or if modifications are required in order to achieve the desired outcomes.
Reducing Biometric Risk and Controlling Disease
If the intent of a wellness program is to help improve the health of individuals so that future medical spending will be reduced, then it is critical to determine if the program is engaging the correct members and then measure the impact on their risk. At Vital Incite, we utilize Johns Hopkins’ risk indexing along with biometric risk migration to provide feedback to vendors and employers of the impact of their programs. Some suggested goals may include:
- Engaging 80 percent of persons with high risk biometrics
- Reduction in weight of persons overweight or obese by greater than 5 percent in 30 percent of the engaged population
- Of diabetics with an A1c greater than 7 percent, 80 percent will reduce their A1c by 1 percent in one year
- Of persons with blood pressure in the high-risk range, 40 percent will have achieved controlled blood pressure without adding medications in one year
- Of persons who take fewer than 10,000 steps per day, 70 percent will increase their average step count by 20 percent or more
These goals need to be very specific and targeted to address the exact needs of your population, measuring what is most likely to have an impact on a person’s long-term health. This provides specific direction for your wellness providers, but allows an employer/consultant to monitor the impact throughout the year to continue to redirect communication and services to help provide the best outcomes.
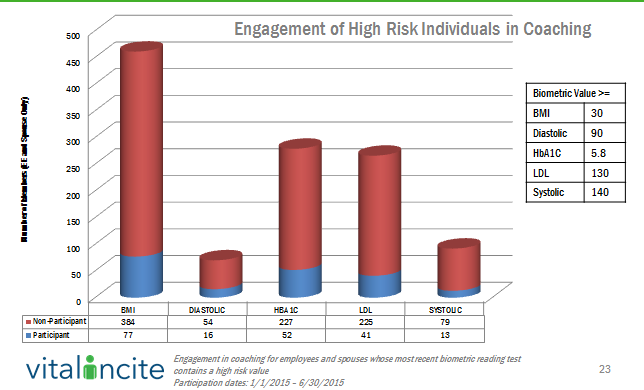
The first step in any program is to engage the intended audience. UBA’s Health Plan Survey finds that 54.6 percent of employers with wellness programs use components such as on-site or telephone coaching for high-risk employees, an increase of 7.5 percent from last year. Once you target the intended audience, engagement of those at risk is critical. Monitoring this subset of data can make sure the vendor resources are directed appropriately and, many times, identify areas where the employer may be able to help.
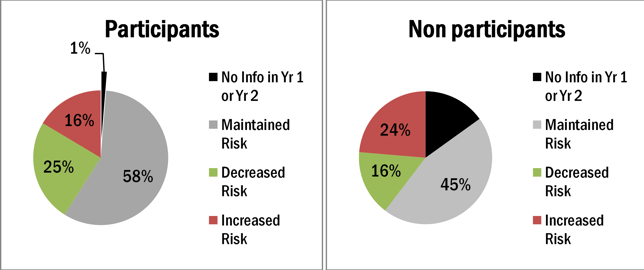
Of course, engagement is only the first step and the intended outcome is to reduce risk or slow down the progression of risk increasing, that is really the final outcome desired. The following illustration allows employers and the vendor solution to monitor the true impact of the program by reviewing the risk control, or improvement based on program participation.
Reducing Medical Spending
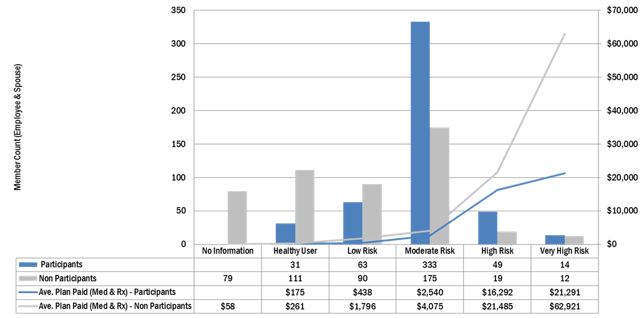
Although many employers are interested in helping their employees become healthier, the reality is these efforts have to help reduce medical costs or increase productivity so these efforts are sustainable. Since, to date, few employers have data on productivity, the analysis then is focused on reducing medical spending. The correct analysis depends on the size of your population and the targeted audience, but a general analysis to determine if those engaged are costing less than persons who have similar risk on your plan would look something like the analysis below.
If your program is targeted specifically on a disease state, then the impact on the cost to care for that disease state may be more appropriate. In the example below, the employer instituted a program to help asthmatics, and therefore, the analysis is related to the total cost to care for asthma comparing the year prior to the program to the year of the program. In this analysis, the impact is very clear.
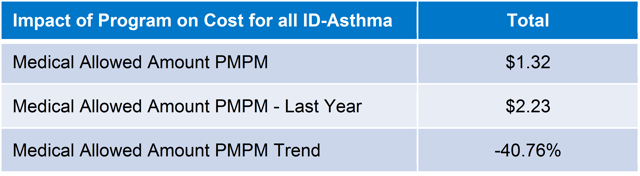
The employer anticipated first year savings due to high emergency room (ER) utilization for persons with asthma and the report proved that along with ER utilization declining, the total cost of care for asthma significantly declined.
Summary
In summary, having a clear understanding of the expectation and desired outcomes and monitoring that impact throughout the year, we believe, drives better outcomes. When we first started analyzing outcomes of programs, the impact of many programs were far less impressive than vendor reports would allow us to believe. That false sense of security is not because they were trying to falsify information, but the reports did not provide enough detail to fully illustrate the impact. Most vendor partners don’t have access to all of the data to provide a full analysis and others will only show what makes them look good. But, if you identify the impact you need in order to achieve success, all parties involved focus on that priority and continually work to improve that impact. We believe that wellness programs can have an impact on a population culture, health and cost of care if appropriately managed.
Download our free (no form!) special report, “2016 Trends in Employer Wellness Programs,” for more information on wellness components trending among employers, especially the increase in telephonic coaching and the decrease in the use of health risk assessments.
For complete health plan design and cost trends by industry, region and group size, download UBA’s 2016 Health Plan Survey Executive Summary.
For comprehensive information on designing wellness programs that create lasting change, download UBA’s whitepaper: “Wellness Programs — Good for You & Good for Your Organization.”
To understand legal requirements for wellness programs, request UBA’s ACA Advisor, “Understanding Wellness Programs and Their Legal Requirements,” which reviews the five most critical questions that wellness program sponsors should ask and work through to determine the obligations of their wellness program under the ACA, HIPAA, ADA, GINA, and ERISA, as well as considerations for wellness programs that involve tobacco use in any way.
By Mary Delaney, Originally published by United Benefit Advisors – Read More
